In nutrition, nothing exists in a vacuum.
Often, diets are defined by adjectives like ‘low’ or ‘high’, however, these words do little to truly inform us about the nature of the diet in question, and its potential health effects.
Digging beyond the level of whole diets, this holds true at the level of nutrients. In fact, this is where the potential health effects of a diet ‘high’ or ‘low’ in any given dietary constituent are determined. In this respect, everything in nutrition is relative, a matter of context.
Recently, a narrative has emerged amongst advocates of low-carb, high fat [‘LCHF’] diets. The narrative runs something like this: in the late 1970’s in the United States, and early 1980’s in the United Kingdom, dietary guidelines were introduced which recommended that people consume less total fat and saturated fat, and this shifted populations to consuming more refined carbs and sugar and, hey presto, we ended up with an obesity epidemic. This narrative is used to suggest that public health nutrition was wrong to focus on saturated fat in the diet, and that as cardiovascular disease remains the leading cause of mortality in the developed world, clearly the fault lies with sugar.
This narrative is wholly misconceived. In the first instance, it is simply wrong: in addition to recommending a reduction in population fat intake, the guidelines also recommended reducing sugar, increasing fiber, vegetables and whole grain carbohydrates [1]. In the interim, sugar has increased, refined carbohydrates predominate in the diet, and fiber and vegetable intake has declined [1][4]. Secondly, but more importantly, it is now acknowledged that while the focus on total fat intake is no longer necessary, the recommendation to decrease saturated fat to 10% of total energy remains valid [2][3].
However, there was one glaring omission in the early dietary guidelines: the guidelines never provided any real advice on what nutrients should replace saturated fat. This is the crux of the issue. The early guidelines are framed in a way that suits the LCHF narrative because the concept of a ‘high’ saturated fat intake, and the health benefits of reducing saturated fat intake, are entirely predicated on what nutrient is displaced or replaced in the diet.
Let’s look at this in more detail. First, some background context.
The Background to Public Health Focus on Saturated Fats
There is another aspect to the narrative framed by the LCHF movement which suggests that the focus was premature and based entirely on flawed epidemiology. This could not be further from the truth. Controlled feeding metabolic ward studies from the 1960’s had demonstrated that, relative to unsaturated fats, dietary saturated fatty acids had the greatest impact on raising LDL-cholesterol [5]. The epidemiology through the 1960’s and 1970’s consistently demonstrated that in certain countries, the saturated fat content in the diet was from 15% to up to 23% total energy [6]. The higher content of saturated fat [SFA] in the diet was strongly, significantly, and consistently associated with heart disease mortality, which was in large part explained by high blood cholesterol levels, in particular LDL-cholesterol [6].
Two crucial points warrant comment here. The first is the suggestion, again heard loudest from the LCHF camp, that LDL-cholesterol is not an issue. This is simply unsupported by the totality of evidence, with the Consensus Panel of the European Atherosclerosis Society recently deeming LDL a “smoking gun” in the pathogenesis of heart disease [7]. In addition, higher LDL levels earlier in life correspond to a greater the risk of heart disease in future [8]. Finally, it is fully accepted in lipidology and cardiovascular disease research that high blood cholesterol levels aren’t the only risk factor for heart disease, and statistically, not all heart disease mortality is associated with elevated cholesterol [9]. However, it remains a significant risk factor overall with substantial predictive value in whole populations [10].
The second point is that the association between SFA, or any nutrient, and a disease outcome – in this case heart disease – is always indirect. The recent suggestions of ‘no association’ between SFA and heart disease are based largely on a misconception that there should be a direct, straight line between SFA and cardiovascular mortality. That will never exist for diet and health outcomes: the effect is always indirect, mediated by the impact on physiological processes like blood cholesterol and atherosclerosis, or inflammation and vascular function.
Taking all of this into consideration, there was nothing inappropriate or incorrect about the historical focus on SFA. It was generated from consistent observations in diverse populations of intakes of saturated fat between 15-23% total energy (the range we mean by “high”) associated with heart disease mortality, mediated by high blood cholesterol levels [6]. It was corroborated by controlled feeding and metabolic ward studies clearly demonstrating that saturated fatty acids had the most negative impact on blood cholesterol compared to unsaturated fats [5]. But when this translated into public health nutrition advice to reduce saturated fats to 10% energy, there was an important omission: what to replace that saturated fat with.
And therein, as Shakespeare would tell it, lies the rub.
The Effects of Replacing Saturated Fat in the Diet
Ironically, it’s not just in the realm of epidemiology that we see associations between high saturated fat intake and CVD: we also see the importance of the replacement nutrient. An interesting observation emerged from a natural experiment in Eastern Europe after the fall of the Soviet Union: a rapid decline in heart disease rates in certain countries, after a period of market transformation and expanding of the food supply [11]. This sharp decline in heart disease mortality was directly correlated with a significant increase in consumption of rapeseed oil, and increased population intake of alpha-linolenic acid [ALA], an omega-3 polyunsaturated fatty acid [PUFA] [11]. Traditionally in Eastern Europe, rapeseed or sunflower oil were the predominant oils, but rapeseed oil had been more expensive and thus animal fats or sunflower oil were consumed in larger amounts before the market turn, two oils which are low in ALA [11]. Market transformation made rapeseed oil more accessible, and its consumption increased significantly in Poland, Latvia, Lithuania, Czech Republic, and Slovakia. These countries with the greatest increase in grams per day of ALA showed the greatest reduction in mortality [11]. In contrast, Russia, Bulgaria and Romania – countries in which sunflower oil remained the primary oil and which showed no increase in ALA – had no change in CVD mortality [11].
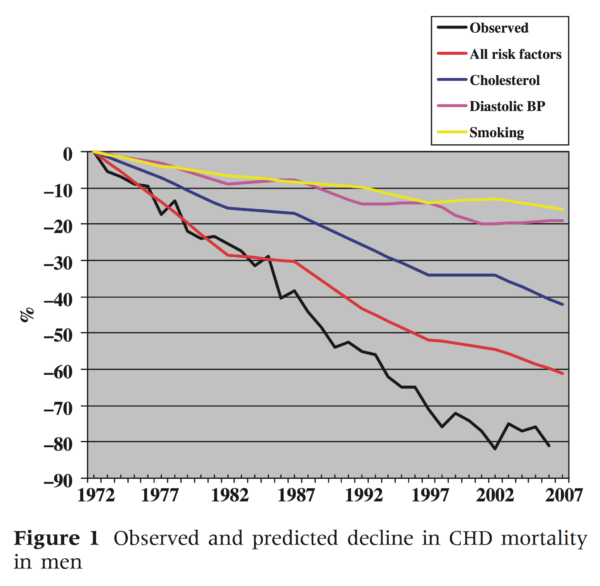
Moving to Northern Europe, of the countries with the highest saturated fat intake in the 1960’s and 1970’s, Finland stood atop the table with the highest population blood cholesterol levels, and experienced the highest CVD mortality globally. Starting in 1972, a targeted public health intervention to reduce CVD mortality targeted specifically reductions in specific risk factors such as blood cholesterol, blood pressure, and smoking. By 2007, CVD mortality had declined by 80% [12], and of the risk factors, population reductions in blood cholesterol accounted for 67% of the decrease in mortality [12]. This reduction in blood cholesterol was in turn attributable to a reduction in saturated fat from 23% to 13%, which was achieved through deliberate public health messaging regarding butter consumption (the most significant contributor to SFA in Finnish diets at the time) [12]. Of particular note, this decrease occurred in the context of smoking rates remaining largely similar, and an overall increase in BMI across the population, both significant risk factors for CVD [12].
This issue of the replacement nutrient and levels of saturated fat in the diet is critical to understanding why several recent meta-analyses all purported to find no association between saturated fat and CVD. In the 2010 meta-analysis which began the controversy, the conclusion that there was no significant association was based on analysis of prospective cohort studies, but the meta-analysis failed to consider the replacement nutrient for saturated fat [13]. A further meta-analysis by the same research group comparing saturated fat to carbohydrate also failed to distinguish between the type – whole grain or refined – of carbohydrate replacing saturated fat [14]. Additional meta-analyses looking at the effects of isolated fatty acids also generated much attention. However, these are wholly uninformative as they failed to account for food sources: people don’t eat individual fatty acids, they eat foods comprised of multiple fatty acids [15][16]. Finally, the recent PURE trial – a large epidemiological study including cohorts from 18 countries –concluded that ‘high’ carbohydrate diets increased CVD mortality and that a ‘high’ saturated fat intake was protective against stroke [17]. This conclusion is a total misnomer: by the authors own admission, they did not differentiate between whole grain and refined carbohydrate [17]. But more erroneous was their conclusion in relation to saturated fat, because the average saturated fat intake overall in the cohorts was 8%, with the US and UK averages around 11-12%. An appropriate conclusion would thus have been: “achieving near target levels of saturated fat in the population has the desired effect of reducing CVD burden, but evidently the type of nutrient replacing saturated fat is relevant as CVD mortality rates remain high.”
These studies indicate that not only is the reduction in total energy from SFA associated with significant population declines in mortality, but that the effect of the nutrient replacing saturated fat is vital also. Let’s look deeper at the replacement nutrients.
Replacing Saturated Fat with Polyunsaturated Fat
This goes first as it is categorically the most protective substitution of one nutrient for another in relation to CVD. The observations noted in Eastern Europe have been found elsewhere. In particular, a meta-analysis of cohort studies looking at ALA found that heart disease mortality reduced by 10% with each 1g/d increase in ALA intake [18]. This has led to the suggestion that in fact, it is specifically PUFA of the omega-3 variety that confer benefit. However, it should be noted that the requirements for omega-3’s are relatively lower, and they constitute a smaller proportion of dietary fat intake [19]. Fish consumption, providing the longer chain omega-3 fatty acids EPA and DHA, is also associated with reduced risk of heart disease in both epidemiology and clinical trials [20]. However, the omega-3 PUFA alone are not sufficient to replace SFA in the diet due to their contributions to health at lower proportions of energy [18], thus the emphasis remains on overall PUFA intake.
This has not been without controversy, as select studies have suggested that omega-6 PUFA in fact increases risk. In particular, the Sydney Diet Heart Study in the late 1960’s and early 1970’s concluded that a 15% omega-6 intake was a greater risk for CVD mortality than SFA intake of <10% energy [21]. However, the intervention used margarine as the source of omega-6’s, which meant subjects were consuming high levels of industrial trans fats [TFA], which profoundly increase risk for heart disease [22]. Accounting for source of omega-6 linoleic acid [LA] is thus important, and the utilization of margarine as a food-based intervention is a significant confounder due to the trans-fat content [18][20][22]. That confounder aside, high dietary intake of omega-6 LA is associated with reduced CVD risk, and meta-analysis of prospective cohort studies examining LA intake found that for each 5% of energy from SFA replaced by LA PUFA, heart disease mortality risk decreased by 13% [20]. Ultimately the totality of research shows that a higher intake of PUFA – inclusive of both omega-6 LA, and omega-3 fatty acids ALA, EPA, and DHA – reduces risk of heart disease [18][19][20][22]. In analysis of both the Nurses’ Health Study cohort and the Health Professional’s Follow-Up Cohort, heart disease mortality was reduced by 25% with isocaloric substitution of 5% PUFA for 5% SFA [22].
All of these associations have been confirmed in randomized, controlled trials. Convincing evidence from RCTs exists to support a lower blood cholesterol level from PUFA-rich diets compared to diets high [20%] in saturated fat, and that the substitution of SFA for PUFA reduces CVD risk [23]. This relationship between PUFA, blood cholesterol levels, and CVD risk is consistently observed in RCTs. In a meta-analysis of controlled feeding studies, the isocaloric replacement of 5% energy from SFA with PUFA reduced LDL-cholesterol by 10mg/dL, and the mean reduction in total cholesterol of 29mg/dL corresponded to a 24% reduction in heart disease risk for each 18mg/dL reduction in TC [24]. Ultimately, the meta-analysis found that for each 5% of energy from SFA replaced by PUFA, CVD risk decreased by 10% [24]. A further meta-analysis of 15 RCTs found that the replacement of SFA with PUFA reduced CVD events by 27% [25] Of particular relevance to the context of nutrients being ‘high’ or ‘low’ in a diet, this meta-analysis demonstrated that reductions in CVD mortality were found where baseline SFA intake was >18%, and where the reduction of SFA was >8% [25]. This is consistent with the totality of the literature.
Consistency across natural experiments, observational epidemiology, and randomised controlled feeding studies renders the strength of evidence for replacing SFA with PUFA robust. While the reduction of SFA per se from higher intakes will reduce heart disease risk, what we see emerging is the degree to which that risk is reduced, relative to the replacement nutrient. Categorically, the replacement of SFA with PUFA has the strongest effect on CVD across the board, from incidence of events to mortality. [18][22][24][25]
Replacing Saturated Fat with Monounsaturated Fats
The replacement of SFA with monounsaturated fats [MUFA] has been clouded somewhat by the fact that MUFA exists in plant sources, but also animal meats and produce. At the level of epidemiology, this has yielded misleading results: in a meta-analysis of 11 cohort studies, the substitution of 5% energy from SFA with MUFA appeared to show a significant and pronounced increase in risk for myocardial infarction [26]. However, this is a misnomer: in the included studies, animal fat was the primary source of MUFA, and prior to trans-fatty acids being distinguished as a sole – and particularly deleterious – subtype, TFA were included within the definition of MUFA [26]. The classification of TFA within the sum of MUFA in part explains the positive associations between replacing SFA with MUFA, and resulting heart disease risk [26].
The other part of the explanation, consistent with a recent move in the field of nutrition science, is that in the reductionist model research often distils down to the isolated nutrient, or even individual fatty acid. Yet, we don’t eat nutrients; we eat foods. The other part of the explanation for the positive associations between MUFA and heart disease in certain cohort studies was that many of the cohorts were in US or Western populations: the MUFA intake in fact reflected a high intake of animal fat and processed foods [16][26]. Given the presence of MUFA in animal fat, high intake of SFA in the diet will often concomitantly have higher energy from MUFA [18][22].
So, how do we tease out the issue with MUFA? First, look to mechanistic effects on risk factors: in a meta-analysis of 60 RCT feeding studies, MUFA have been shown to lower LDL, lower triglycerides, and improve the total cholesterol to HDL [TC:HDL] ratio [27]. This improvement of lipid profiles is, however, second to PUFA when we look at LDL and triglycerides in particular, which underlies the protective effect of PUFA [24][27]. However, there is one aspect of lipid profiles where MUFA exceed PUFA: raising HDL-cholesterol [28]. However, as MUFA raise HDL more than PUFA, but PUFA lower LDL to a greater degree, the effect on the TC:HDL ratio when either unsaturated fat type replace saturated fat is comparable [28][29]. From the perspective of risk factors, it is clear from the overall body of literature that the isocaloric replacement of SFA with MUFA improves lipid profiles across the board [29].
This has played out in epidemiology, with replacement of 5% energy from SFA with 5% from plant-sourced MUFA associated with a significant reduction in heart disease risk [22]. In March of 2018, an analysis of the Nurses Health Study and Health Professionals Follow-Up Study demonstrated that replacement of 5% of the sum of SFA and animal-based MUFA with plant-based MUFA lowered heart disease risk by 19%, and the substitution of animal-MUFA for plant-MUFA lowered risk by 24% [30]. These observations corroborate the findings in previous population cohorts of increased risk associated with a higher animal fat consumption [26][30]. More particularly, this finding highlights the importance of the emerging ‘food-first’ paradigm in nutrition research, and where the focus on foods, not nutrients, emerges to help clarify the situation with MUFA.
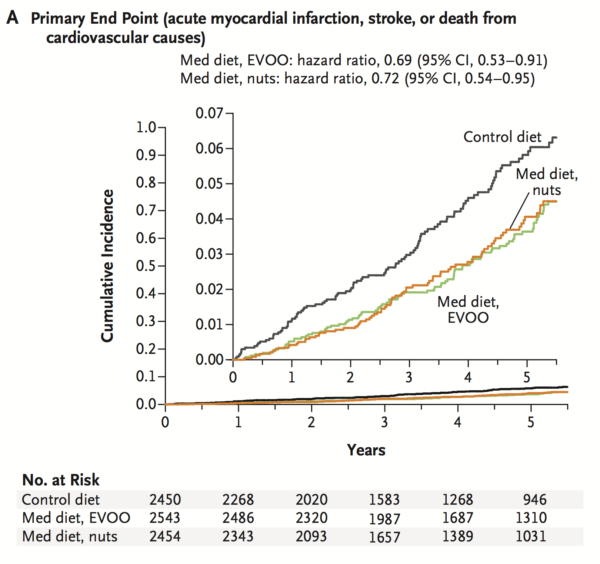
In perhaps one of the best known trials in nutrition, the PREDIMED study in Spain randomised patients at risk of cardiovascular disease to consume either a Mediterranean diet supplemented with 4-tablespoons extra-virgin olive oil per day or a Mediterranean diet supplemented with 30g of mixed nuts (walnuts, hazelnuts, and almonds) daily, compared to a control diet with advice to reduce total fat [31]. A feature of the intervention groups was that neither caloric restriction or physical activity was prescribed, yet at 5-years follow-up the intervention diets had a 30% lower risk of cardiovascular disease compared to controls [31]. The effects of the MUFA-rich intervention diets must be judged in the context of subjects in these groups increasing total fat intake by 5%, to 45% total energy [31]. Consistent with the current position in nutrition, the total fat content of the diet is no longer considered relevant for health outcomes, however, the composition of the fats in the diet is. Of particular note, analysis of PREDIMED still found that saturated fat were adversely associated with metabolic risk factors [32].
Replacing Saturated Fat with Carbohydrate
This has also been an area of controversy of late, given the modern scapegoat for all current lifestyle disease has been dietary carbohydrates. However, like MUFA, closer scrutiny of this issue reveals a distinct and divergent effect of carbohydrate quality – whole grain or refined – as the replacement nutrient for saturated fats.
Certain epidemiological studies have concluded that replacing saturated fat with carbohydrate either has no effect on lifestyle disease risk, or in fact increases it [14][17]. However, these studies failed to distinguish between carbohydrate type. This is a critical omission, as the effects of replacing saturated fat with either whole grain or refined carbohydrates are oppositional. The fact that the norm in population cohorts is replacement of saturated fat with refined grains and added sugars in large part explains why many recent meta-analyses have concluded that there is no association between saturated fat and heart disease [18][22].
Accounting for carbohydrate type, analysis of the Nurses’ Health Study and Health Professionals Follow-Up Study found that replacing 5% energy from SFA with whole grain carbohydrate decreased heart disease risk by 23% after adjusting for confounders [22]. Conversely, replacing the SFA with refined grains and added sugars resulted in risk remaining the same [22]. One way of assessing this is through use of the glycemic index: while it is not particularly informative about a given food or meal in isolation, it is a useful tool at a population level as a reflection of carbohydrate quality of the diet. In analysis of the effects of replacing SFA with carbohydrate classified according to GI, there was no change in myocardial infarction risk with low-medium, but 33% increase in risk where high GI carbs replaced SFA [33].
This indicates the central position of carbohydrate quality in modulating heart disease risk, particularly when substituting for SFA in the diet. Wholegrain carbohydrates, due to their fibre and phytochemical properties in the bran, endosperm, and germ, reduce LDL cholesterol, improve post-prandial blood glucose responses, and increase whole-body insulin sensitivity [34][35][36][37]. Correspondingly, in reducing the contribution of energy from SFA in the diet, replacing that energy with carbohydrates from whole grain sources significantly reduces risk of heart disease [18][22][34][37]. That the primary replacement nutrient for SFA in population diets has been refined grains and added sugars, which do not alter risk, should not – as many in the LCHF paradigm attempt to portray – be taken to mean that SFA are not an issue.
Nutrition in Context
Looking at the effects of a given nutrient in the diet in isolation is the very manifestation of the old adage, ‘failing to see the forest for the trees’. If we consider any given nutrient ‘high’ or ‘low’ in the diet, the relevant question is what is being displaced or replaced as a result of an increase or decrease of a nutrient. It is always relative. And so it is with saturated fats, and the context in which a ‘high’ [>15% energy] saturated fat diet was and potentially is problematic.
The early associations between SFA and CVD were relative to intakes of SFA of 15-25% energy. Reducing risk of heart disease across populations from dietary change is relative to a high SFA intake at baseline, and relative to achieving a reduction of total SFA to 10%. And because we eat food, the health effects of reducing anything in the diet are relative to what foods – and the nutrients they contain – replace the previous energy.
When it comes to the issue of saturated fat and cardiovascular health, the purpose of the desired reduction to 10% energy is due to the clear reduction in total cardiovascular events observed with a decrease to that threshold [38][39]. The question is, to what extent is health served by the various options for replacement nutrients? An overall analysis of the literature reveals a clear hierarchy and the most pronounced reductions in cardiovascular risk occur when SFA are substituted for:
- Polyunsaturated fats;
- Plant-based monounsaturated fats;
- Unrefined, whole grain carbohydrates;
[18][22][24][25][27][28][29][30][31][38][39].

This is an important point in view of the narrative from the LCHF paradigm that saturated fats are not harmful. Even if we take their case at its highest, that SFA are not harmful or benign, they still remain the least healthful option for increasing a nutrient in your diet. The only exception is refined grains/added sugars, and trans-fats. However, the latter is a moot point as they have largely been removed from the food supply. And categorically, there is no evidence of benefit to increasing saturated fats in the diet if they are within target range of ≤10% energy [39].
It is also important to reinforce that we are no longer focused on reducing total fat intake in population diets, but in modifying the composition of those fats to one which reflects the evidence base for dietary fat: a diet with predominantly unsaturated fats [40]. Every level of evidence – epidemiology, controlled feeding studies with risk factor endpoints, and food-based RCT’s with hard clinical endpoints – supports this position.
In the context of food-based recommendations, let’s end with this statement: we know what diet patterns maximally benefit human health. Those diet patterns are high in unsaturated fats from fish, nuts, seeds, and vegetable oils like extra-virgin olive oil or rapeseed oil, they are high in complex carbohydrates from legumes (lentils, chickpeas, various beans) and whole grains (oats, bulgar, couscous, pasta, polenta, and breads from whole grain sources), they are rich in a variety of non-starchy vegetables, and include plenty of fruit. Movements in nutrition that mount spurious claims about diet and health obscure the simplicity of this truth.
References
- Foster R, Lunn J. 40th Anniversary Briefing Paper: Food availability and our changing diet. Nutrition Bulletin. 2007;32(3):187-249.
- U.S. Department of Health and Human Services and U.S. Department of Agriculture. 2015 – 2020 Dietary Guidelines for Americans. 2015.
- The Swedish National Food Agency. Find your way to eat greener, not too much and to be active!. The Swedish National Food Agency; 2015.
- Nielsen S, Siega-Riz A, Popkin B. Trends in Energy Intake in U.S. between 1977 and 1996: Similar Shifts Seen across Age Groups. Obesity Research. 2002;10(5):370-378.
- Clarke R, Frost C, Collins R, Appleby P, Peto R. Dietary lipids and blood cholesterol: quantitative meta-analysis of metabolic ward studies. BMJ. 1997;314(7074):112-112.
- Kromhout D, Menotti A, Bloemberg B, Aravanis C, Blackburn H, Buzina R et al. Dietary Saturated and transFatty Acids and Cholesterol and 25-Year Mortality from Coronary Heart Disease: The Seven Countries Study. Preventive Medicine. 1995;24(3):308-315.
- Ference B, Ginsberg H, Graham I, Ray K, Packard C, Bruckert E et al. Low-density lipoproteins cause atherosclerotic cardiovascular disease. 1. Evidence from genetic, epidemiologic, and clinical studies. A consensus statement from the European Atherosclerosis Society Consensus Panel. European Heart Journal. 2017;38(32):2459-2472.
- Ference B, Yoo W, Alesh I, Mahajan N, Mirowska K, Mewada A et al. Effect of Long-Term Exposure to Lower Low-Density Lipoprotein Cholesterol Beginning Early in Life on the Risk of Coronary Heart Disease. Journal of the American College of Cardiology. 2012;60(25):2631-2639.
- Castelli W. Lipids, risk factors and ischaemic heart disease. Atherosclerosis. 1996;124:S1-S9.
- Khot U, Khot M, Bajzer C. Prevalence of conventional risk factors in patients with coronary heart disease. ACC Current Journal Review. 2003;12(6):23.
- Zatonski W, Campos H, Willett W. Rapid declines in coronary heart disease mortality in Eastern Europe are associated with increased consumption of oils rich in alpha-linolenic acid. European Journal of Epidemiology. 2007;23(1):3-10.
- Vartiainen E, Laatikainen T, Peltonen M, Juolevi A, Mannisto S, Sundvall J et al. Thirty-five-year trends in cardiovascular risk factors in Finland. International Journal of Epidemiology. 2009;39(2):504-518.
- Siri-Tarino P, Sun Q, Hu F, Krauss R. Meta-analysis of prospective cohort studies evaluating the association of saturated fat with cardiovascular disease. The American Journal of Clinical Nutrition. 2010;91(3):535-546.
- Siri-Tarino P, Sun Q, Hu F, Krauss R. Saturated Fatty Acids and Risk of Coronary Heart Disease: Modulation by Replacement Nutrients. Current Atherosclerosis Reports. 2010;12(6):384-390.
- Chowdhury R, Warnakula S, Kunutsor S, Crowe F, Ward H, Johnson L et al. Association of Dietary, Circulating, and Supplement Fatty Acids With Coronary Risk. Annals of Internal Medicine. 2014;160(6):398.
- de Souza R, Mente A, Maroleanu A, Cozma A, Ha V, Kishibe T et al. Intake of saturated and trans unsaturated fatty acids and risk of all cause mortality, cardiovascular disease, and type 2 diabetes: systematic review and meta-analysis of observational studies. BMJ. 2015;:h3978.
- Dehghan M, Mente A, Zhang X, Swaminathan S, Li W. Associations of fats and carbohydrate intake with cardiovascular disease and mortality in 18 countries from five continents (PURE): a prospective cohort study. Lancet. 2017;390:2050–62.
- Pan A, Chen M, Chowdhury R, Wu J, Sun Q, Campos H et al. α-Linolenic acid and risk of cardiovascular disease: a systematic review and meta-analysis. The American Journal of Clinical Nutrition. 2012;96(6):1262-1273.
- Briggs M, Petersen K, Kris-Etherton P. Saturated Fatty Acids and Cardiovascular Disease: Replacements for Saturated Fat to Reduce Cardiovascular Risk. Healthcare. 2017;5(2):29.
- Kris-Etherton P, Fleming J. Emerging Nutrition Science on Fatty Acids and Cardiovascular Disease: Nutritionists’ Perspectives. Advances in Nutrition. 2015;6(3):326S-337S.
- Ramsden C, Zamora D, Leelarthaepin B, Majchrzak-Hong S, Faurot K, Suchindran C et al. Use of dietary linoleic acid for secondary prevention of coronary heart disease and death: evaluation of recovered data from the Sydney Diet Heart Study and updated meta-analysis. BMJ. 2013;346(feb04 3):e8707-e8707.
- Li Y, Hruby A, Bernstein A, Ley S, Wang D, Chiuve S et al. Saturated Fats Compared With Unsaturated Fats and Sources of Carbohydrates in Relation to Risk of Coronary Heart Disease. Journal of the American College of Cardiology. 2015;66(14):1538-1548.
- Schwab U, Lauritzen L, Tholstrup T, Haldorsson T, Riserus U, Uusitupa M et al. Effect of the amount and type of dietary fat on cardiometabolic risk factors and risk of developing type 2 diabetes, cardiovascular diseases, and cancer: a systematic review. Food & Nutrition Research. 2014;58(1):25145.
- Mozaffarian D, Micha R, Wallace S. Effects on Coronary Heart Disease of Increasing Polyunsaturated Fat in Place of Saturated Fat: A Systematic Review and Meta-Analysis of Randomized Controlled Trials. PLoS Medicine. 2010;7(3):e1000252.
- Hooper L, Martin N, Abdelhamid A, Davey Smith G. Reduction in saturated fat intake for cardiovascular disease. Cochrane Database of Systematic Reviews. 2015;.
- Jakobsen M, O’Reilly E, Heitmann B, Pereira M, Bälter K, Fraser G et al. Major types of dietary fat and risk of coronary heart disease: a pooled analysis of 11 cohort studies. The American Journal of Clinical Nutrition. 2009;89(5):1425-1432.
- Mensink R, Zock P, Kester A, Katan M. Effects of dietary fatty acids and carbohydrates on the ratio of serum total to HDL cholesterol and on serum lipids and apolipoproteins: a meta-analysis of 60 controlled trials. The American Journal of Clinical Nutrition. 2003;77(5):1146-1155.
- Hodson L, Skeaff C, Chisholm W. The effect of replacing dietary saturated fat with polyunsaturated or monounsaturated fat on plasma lipids in free-living young adults. European Journal of Clinical Nutrition. 2001;55(10):908-915.
- Gillingham L, Harris-Janz S, Jones P. Dietary Monounsaturated Fatty Acids Are Protective Against Metabolic Syndrome and Cardiovascular Disease Risk Factors. Lipids. 2011;46(3):209-228.
- Zong G, Li Y, Sampson L, Dougherty L, Willett W, Wanders A et al. Monounsaturated fats from plant and animal sources in relation to risk of coronary heart disease among US men and women. The American Journal of Clinical Nutrition. 2018;107(3):445-453.
- Estruch R, Ros E, Salas-Salvadó J, Covas M. Primary Prevention of Cardiovascular Disease with a Mediterranean Diet Supplemented with Extra-Virgin Olive Oil or Nuts. N Engl J Med. 2018;378(e34).
- Mayneris-Perxachs J, Sala-Vila A, Chisaguano M, Castellote A, Estruch R, Covas M et al. Effects of 1-Year Intervention with a Mediterranean Diet on Plasma Fatty Acid Composition and Metabolic Syndrome in a Population at High Cardiovascular Risk. PLoS ONE. 2014;9(3):e85202.
- Jakobsen M, Dethlefsen C, Joensen A, Stegger J, Tjønneland A, Schmidt E et al. Intake of carbohydrates compared with intake of saturated fatty acids and risk of myocardial infarction: importance of the glycemic index. The American Journal of Clinical Nutrition. 2010;91(6):1764-1768.
- Flight I, Clifton P. Cereal grains and legumes in the prevention of coronary heart disease and stroke: a review of the literature. European Journal of Clinical Nutrition. 2006;60(10):1145-1159.
- Venn B, Mann J. Cereal grains, legumes and diabetes. European Journal of Clinical Nutrition. 2004;58(11):1443-1461.
- Pereira M, Jacobs D, Pins J, Raatz S, Gross M, Slavin J et al. Effect of whole grains on insulin sensitivity in overweight hyperinsulinemic adults. The American Journal of Clinical Nutrition. 2002;75(5):848-855.
- Kirwan J, Malin S, Scelsi A, Kullman E, Navaneethan S, Pagadala M et al. A Whole-Grain Diet Reduces Cardiovascular Risk Factors in Overweight and Obese Adults: A Randomized Controlled Trial. The Journal of Nutrition. 2016;146(11):2244-2251.
- Scientific Advisory Committee on Nutrition. Saturated fats and health. Public Health England; 2018.
- World Health Organisation. Guidelines: Saturated fatty acid and trans-fatty acid intake for adults and children. WHO; 2018.
- Mozaffarian D. Dietary and Policy Priorities for Cardiovascular Disease, Diabetes, and Obesity. Circulation. 2016;133(2):187-225.


